22q11.2 deletion: the most common syndrome you have never heard of
4 June 2019
Hayley Moulding, School of Medicine
You wouldn’t be blamed for thinking that 22q11.2 was a postcode or password. My guess is you wouldn’t have thought it was the most prevalent syndrome of its kind.
So let’s talk about “22q”.
Everyone has 23 pairs of chromosomes – that’s 46 all together. Chromosomes are made of genes, which themselves are built of DNA. Think of a chromosome as a complete puzzle: the genes are the individual pieces and the DNA is the pattern or picture. When the different pieces are fixed together, they create a complete chromosome. In people with a genetic syndrome like 22q, a piece of the puzzle is missing, leaving the picture incomplete.
In 22q, the missing section is found on the “q arm” of the 22nd chromosome, at a position identified as 11.2 which combined becomes 22q11.2. The missing section can differ in size, meaning people can experience different symptoms. However, there is a core region commonly deleted in all.
The prevalence of 22q is considered to be around one in 2,000 live births globally. This number is constantly under review however, with the syndrome potentially more common than initially thought. Many people go through life without a diagnosis.
What problems occur in 22q?
Because of the myriad problems in 22q, many different specialists are involved in diagnosing and treating it. It doesn’t help that different specialists refer to 22q by different names such as DiGeorge syndrome, or velocardiofacial syndrome. These share a 22q deletion yet are considered different syndromes. In my world of research however, we talk about it as “22q”.
When a diagnosis is first made, the focus is commonly on the physical effects of the syndrome, such as cleft palate and heart defects. These effects are of course dependent on when and why a diagnosis was sought or given. Some diagnoses occur because of behavioural or developmental problems – autism-like symptoms or inattention and hyperactivity, for example – not just physical. These developmental and psychiatric problems come with age but can be traced back to earlier years.
22q has one of the highest prevalences of developmental delay and congenital heart disease, second only to Down’s syndrome. Further similarities include both having a broad range of symptoms – including poor muscle tone and differences in digit length, both fingers and toes – and facial features. These tend to be more stereotyped in Down’s syndrome, but can be evident in 22q.
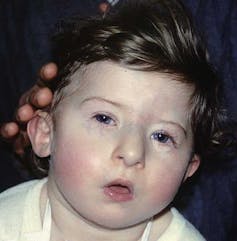
Prof Victor Grech/Wikimedia, CC BY-SA
22q also puts individuals at increased risk of schizophrenia. In the general population, 1-2% of people have schizophrenia. In 22q, this rate is higher, at around 25-30% of people. 22q is one of the highest implicated genetic changes of its kind for development of schizophrenia. Strikingly, this elevated risk is higher than having one parent with schizophrenia, which is 10%. Having such a pronounced and stigmatised disorder at this risk level highlights the need for more understanding of 22q, as well as better interventions and treatments.
Other psychiatric disorders are more prevalent in 22q as well, including anxiety disorders, attention-deficit hyperactivity disorder (ADHD) and autism. Epilepsy and impaired motor coordination are also common.
One of the most uncharted problems of 22q is that of sleep disturbances, which is what I am currently researching. Some people with 22q have physical sleep-related problems such as obstructive sleep apnoea, however sleep-related behavioural and psychological problems have yet to be fully investigated.
How people with 22q sleep, both from a physiological view of brain activity to comfort and restlessness, can open the doors to understanding more about 22q as a multiplex syndrome. My work involves assessing children and adolescents’ brain activity during a night’s sleep. Coupling electroencephalography (EEG), which records electrical activity in the brain, with other objective sleep measures, can help us to create a better picture of what sleep is like in 22q.
Why is 22q important?
Families taking part in our research give a brief window into their lives, and we get snippets of the day-to-day realities of living with the syndrome. Although I would never claim to know what it’s like to have a child or be an adult with 22q, I greatly sympathise with the problems they experience.
Immediate life threatening heart defects at birth, and developmental delay and sensory processing problems can aggregate in childhood. The emergence of hallucinations and delusions in early adolescence can manifest into schizophrenia and anxiety, which can have a debilitating impact in adulthood.
Dealing with each of these problems separately takes a lot of strength and perseverance on the part of a person and their family. The cocktail of problems faced everyday makes for a hard pill to swallow and are difficult to ignore.
However, society’s lack of awareness is unhelpful: having to explain yourself day after day, being stigmatised, judged, or confronted with a face of confusion and lack of empathy must be beyond unbearable.
Researchers like myself are working hard to make sure 22q is investigated, taught, and discussed more widely, so that people and their families who are affected are given the understanding they deserve.![]()
Hayley Moulding, PhD student in Neuropsychiatric Genetics and Genomics, Cardiff University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Comments
1 comment
Comments are closed.
- June 2024
- March 2024
- February 2024
- November 2023
- September 2023
- June 2023
- May 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- July 2022
- May 2022
- April 2022
- January 2022
- December 2021
- November 2021
- August 2021
- July 2021
- June 2021
- February 2021
- January 2021
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- Biosciences
- Careers
- Conferences
- Development
- Doctoral Academy Champions
- Doctoral Academy team
- Events
- Facilities
- Funding
- Humanities
- Internships
- Introduction
- Mental Health
- PGR Journeys
- Politics
- Public Engagement
- Research
- Sciences
- Social Sciences
- Staff
- STEM
- Success Stories
- Top tips
- Training
- Uncategorized
- Wellbeing
- Working from home
This is great, such an interesting and so important to raise awareness of 22q11-2-deletion: https://fdna.health/syndromes/22q11-2-deletion-syndrome/