Coronavirus nanoscience: the tiny technologies tackling a global pandemic
9 October 2020Josh Davies, School of Chemistry
The world-altering coronavirus behind the COVID-19 pandemic is thought to be just 60 nanometres to 120 nanometres in size. This is so mind bogglingly small that you could fit more than 400 of these virus particles into the width of a single hair on your head. In fact, coronaviruses are so small that we can’t see them with normal microscopes and require much fancier electron microscopes to study them. How can we battle a foe so minuscule that we cannot see it?
One solution is to fight tiny with tiny. Nanotechnology relates to any technology that is or contains components that are between 1nm and 100nm in size. Nanomedicine that takes advantage of such tiny technology is used in everything from plasters that contain anti-bacterial nanoparticles of silver to complex diagnostic machines.
Nanotechnology also has an impressive record against viruses and has been used since the late 1880s to separate and identify them. More recently, nanomedicine has been used to develop treatments for flu, Zika and HIV. And now it’s joining the fight against the COVID-19 virus, SARS-CoV-2.
Diagnosis
If you’re suspected of having COVID, swabs from your throat or nose will be taken and tested by reverse transcription polymerase chain reaction (RT-PCR). This method checks if genetic material from the coronavirus is present in the sample.
Despite being highly accurate, the test can take up to three days to produce results, requires high-tech equipment only accessible in a lab, and can only tell if you have an active infection when the test is taken. But antibody tests, which check for the presence of coronavirus antibodies in your blood, can produce results immediately, wherever you’re tested.
Antibodies are formed when your body fights back against a virus. They are tiny proteins that search for and destroy invaders by hunting for the chemical markers of germs, called antigens. This means antibody tests can not only tell if you have coronavirus but if you have previously had it.
Antibody tests use nanoparticles of materials such as gold to capture any antibodies from a blood sample. These then slowly travel along a small piece of paper and stick to an antigen test line that only the coronavirus antibody will bond to. This makes the line visible and indicates that antibodies are present in the sample. These tests are more than 95% accurate and can give results within 15 minutes.
Vaccines and treatment
A major turning point in the battle against coronavirus will be the development of a successful vaccine. Vaccines often contain an inactive form of a virus that acts as an antigen to train your immune system and enable it develop antibodies. That way, when it meets the real virus, your immune system is ready and able to resist infection.
But there are some limitations in that typical vaccine material can prematurely break down in the bloodstream and does not always reach the target location, reducing the efficiency of a vaccine. One solution is to enclose the vaccine material inside a nanoshell by a process called encapsulation.
These shells are made from fats called lipids and can be as thin as 5nm in diameter, which is 50,000 times thinner than an egg shell. The nanoshells protect the inner vaccine from breaking down and can also be decorated with molecules that target specific cells to make them more effective at delivering their cargo.
This can improve the immune response of elderly people to the vaccine. And critically, people typically need lower doses of these encapsulated vaccines to develop immunity, meaning you can more quickly produce enough to vaccinate an entire population.
Encapsulation can also improve viral treatments. A major contribution to the deaths of virus patients in intensive care is “acute respiratory distress syndrome”, which occurs when the immune system produces an excessive response. Encapsulated vaccines can target specific areas of the body to deliver immunosuppressive drugs directly to targeted organs and helping regulate our immune system response.
Transmission reduction
It’s hard to exaggerate the importance of wearing face masks and washing your hands to reducing the spread of COVID-19. But typical face coverings can have trouble stopping the most penetrating particles of respiratory droplets, and many can only be used once.
New fabrics made from nanofibres 100nm thick and coated in titanium oxide can catch droplets smaller than 1,000nm and so they can be destroyed by ultraviolet (UV) radiation from sunlight. Masks, gloves and other personal protective equipment (PPE) made from such fabrics can also be washed and reused, and are more breathable.
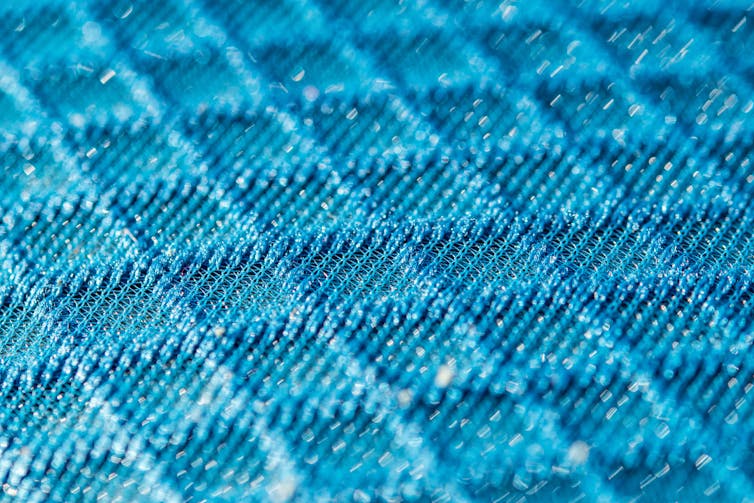
Another important nanomaterial is graphene, which is formed from a single honeycomb layer of carbon atoms and is 200 times stronger than steel but lighter than paper. Fabrics laced with graphene can capture viruses and block them from passing through. PPE containing graphene could be more puncture, flame, UV and microbe resistant while also being light weight.
Graphene isn’t reserved for fabrics either. Nanoparticles could be placed on surfaces in public places that might be particularly likely to facilitate transmission of the virus.
These technologies are just some of the ways nanoscience is contributing to the battle against COVID-19. While there is no one answer to a global pandemic, these tiny technologies certainly have the potential to be an important part of the solution.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
- February 2025
- September 2024
- June 2024
- March 2024
- February 2024
- November 2023
- September 2023
- June 2023
- May 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- July 2022
- May 2022
- April 2022
- January 2022
- December 2021
- November 2021
- August 2021
- July 2021
- June 2021
- February 2021
- January 2021
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- Biosciences
- Careers
- Conferences
- Development
- Doctoral Academy Champions
- Doctoral Academy team
- Events
- Facilities
- Funding
- Humanities
- Internships
- Introduction
- Mental Health
- PGR Journeys
- Politics
- Public Engagement
- Research
- Sciences
- Social Sciences
- Staff
- STEM
- Success Stories
- Top tips
- Training
- Uncategorized
- Wellbeing
- Working from home