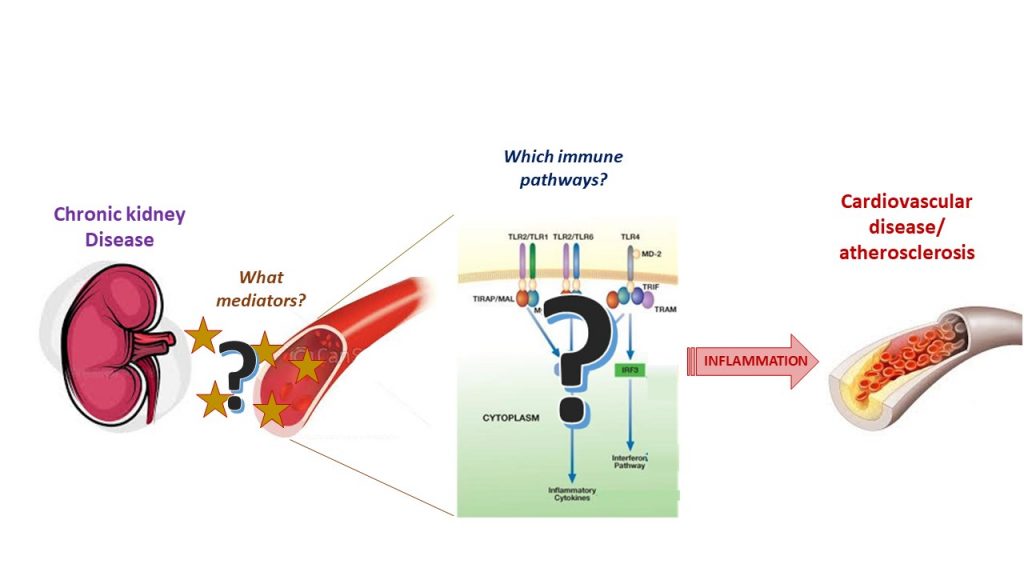
Searching for the ‘missing link’ between kidney disease and cardiovascular disease
16 December 2020Dr Anne-Catherine Raby is a researcher at the School of Medicine, looking for the link between chronic kidney disease and cardiovascular disease with a focus on inflammation. Her work is far-reaching, all-consuming, and imperative in understanding the disease responsible for more deaths globally than any other cause.
Sometimes, I want to say this research path chose me.
I’ve been working on a particular family of receptors involved in inflammation since my master’s thesis, and inflammation plays such a significant role in kidney disease and cardiovascular disease (CVD), that it was a natural progression.
Research in this area is vital because CVD is the number one cause of death globally, with roughly 80 million people dying of a CVD-related condition every year. It is an umbrella term that covers conditions of the heart, the vessels, and the circulation.
Unfortunately, it will affect all of us, either directly or through a loved one.
But there are good indications that aspects of CVD are changeable. Three quarters of CVD deaths occur in low to middle income countries, suggesting that environment and healthcare options can make a difference. Early management and detection contribute to better outcomes and so we must keep looking for answers, for anything that can make a difference.
CVD, inflammation and kidney disease: finding the connection
It is well accepted in the research community that there is a strong link between some types of CVD and inflammation, but it is not well explained. We can detect inflammatory markers in the blood that either correlate with an underlying CVD condition or correlate with the prognosis.
It is a case of the chicken or the egg; we don’t know if inflammation is the cause of CVD conditions, or if it’s the consequence, or if it’s both! But it means that, potentially, inflammation is a very good target for treatment.
As well as a connection with inflammation, there is a strong link between the heart and the kidneys. This is known as cardiorenal syndrome.
If you smoke or are obese, this can increase your risk of both kidney disease and CVD, and it’s not surprising to find the two diseases in the same people. If your blood pressure is too high that can damage the kidneys. If the kidneys fail, they won’t remove water from your system and your blood pressure increases, which in turn is a problem for the heart. And when you add inflammation into the mix, it can induce problems for both.
Why our research has the potential to be game changing
Our work is heavily based in the laboratory. We do experiments with test tubes, for example using cells from patients and also conduct in vivo experiments. We look at blood from different patients and compare them for levels of particular mediators of inflammation. We have so far found four mediators that are present at higher levels in patients with chronic kidney disease than those of healthy individuals. We have exposed healthy blood cells to these mediators to see if it would induce the healthy samples to behave in the same way. So far, we have found that two of them can indeed make cells behave in a way that promotes the narrowing of the arteries.
Some aspects of CVD and kidney disease we can change, and some we cannot. We need to know which things to target and what will improve outcomes. Our hypothesis is that inflammation coming from the kidneys in those with kidney disease worsens CVD development. If we can prove this, we then need to figure out if blocking inflammation is enough to reduce issues. The results could then be turned into something that can be administered either as a prevention, or to block the formation of CVD once it has already begun. The implications of this are fantastic and game changing.
There is the possibility that if this applies to one condition, it could be applied to others that work in similar ways. Diseases tend to cluster together in the same individuals, known as ‘multimorbidity’. If this hypothesis is correct, the aim would be to expand this into the context of other morbidities associated with CVD or kidney disease such as diabetes, dementia and arthritis.
The best part of my job is when my experiments generate many pieces of information that I can’t make sense of and I’m trying to figure it out – like a puzzle. Gradually, you start seeing a picture and it starts to make sense. You don’t get a lot of ‘eureka’ moments but sometimes you get results that you know will be game changers. Putting the pieces together is definitely the best part of my job.
Vital funding and the generosity of British people
This research would not be possible without funding – it makes all the difference. I received my lectureship through Wales Heart Research Institute, and this has allowed me to do this important work. We can spend a year looking for funding and, realistically, this takes your focus away from the research. It can be very disruptive and discourages lots of talented early-career researchers. The implications of receiving funding is that I can continue with my research and transition to a long-term contract and can focus completely on the research. I have two PhD students and I can supervise them without thinking about having to reapply for money in six months. It takes the pressure off and puts me in the best possible position to start building on the research, which can then help me leverage more funding in the future.
Donating money is a very personal thing and funding needs to go everywhere, but for those who support research, please be assured that your support is invaluable. I’m always impressed by the generosity of British people. I’ve worked in several countries, but I’ve never seen charities receive such welcome and funding on this scale. British people are very generous!
Find out more about how you can support Cardiff University’s research.
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- November 2016
- October 2016
- September 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- January 2015
- December 2014
- November 2014
- September 2014
- August 2014
- May 2014