Our PrEP Research And What It Means To Wales (And Beyond)
4 July 2020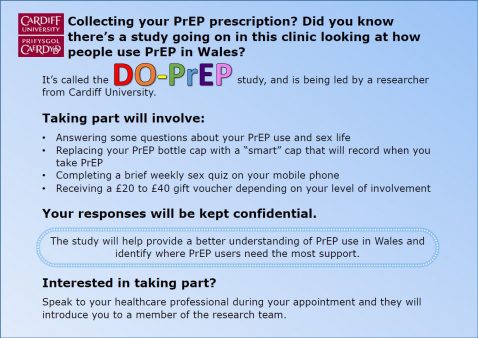
Background
A few days ago, the Welsh Cabinet Secretary for Health, Vaughan Gething, announced that the use of pre-exposure prophylaxis (known as PrEP) to prevent HIV would become routine in the NHS in Wales following assessment by the All Wales Medicines Strategy Group (AWMSG). This follows a three year research evaluation after the AWMSG had previously determined that the routine provision of PrEP was not cost effective. It is fair to say that the announcement of the three year evaluation came as a surprise and I can still remember the disappointed and outraged discussions on social media following the AWMSGs previous assessment. Despite the results of the PROUD Trial which had been stopped early due to the effectiveness of the medication, there seemed to be two issues driving the cost effectiveness assessment – the cost of the drug and some concern about adherence. Of course wrapped around this was a perception that there was an inequality and bias against people who were at risk of acquiring HIV.
Role Of Well-Designed Studies
From a Centre perspective we had a track record of designing and evaluating interventions for the management of infections, including a focus on individual and health professional behaviour. Within a few hours of Vaughan Gething’s announcement in 2017 I contacted everyone I could think of to find out what form the research in Wales would take. This led me to meeting Zoe Couzens and Adam Jones from Public Health Wales who were leading on rolling out the service across Wales. Over a lengthy cup of coffee in a hotel foyer, we shaped out a vision of what a more extensive research programme could look like and the really important questions for us to answer in Wales. Two of the areas we identified for further work were a concern of mine that effective drugs might not be recommended due to adherence issues, when what needed to happen was to improve adherence and the other was a concern of Zoe and Adam’s that rates of sexually transmitted infections could be attributed to assumed reduced condom use. This has led to a partnership which has resulted in a Research Fellowship for Dr David Gillespie to study adherence in the Welsh PrEP users population (DO-PREP) and a PhD studentship for Adam Williams to study the links between PrEP use, condom use and sexually transmitted infections.
Health and Care Research Wales Funded Fellowship Investigates Adherence To PrEP Use

As a medicine used to prevent HIV, “adherence” to PrEP requires consideration not only of medicine use but also of periods of risk exposure, which are not fixed permanent states but can fluctuate over time. Dave’s fellowship was funded by Health and Care Research Wales, as part of the Health Research Fellowship scheme. From October 2018 (just over a year into the initial roll out of PrEP in Wales), and over a 5-year period, Dave is investigating how individuals accessing PrEP through sexual health clinics in Wales are using it, how their use corresponds to their sexual behaviour (as this is the primary route of HIV transmission), and whether there are any processes that influence sub-optimal use of PrEP. He is currently conducting a 9-month intensive longitudinal study, using electronic medicine caps to measure PrEP use, and weekly electronic surveys to measure sexual behaviour, and an embedded qualitative study where participants will be interviewed about their experiences of using PrEP. He hopes to use data from these studies, as well as a comprehensive review of relevant literature around adherence to PrEP and other similar preventative medicines, to develop a prototype intervention to improve how PrEP is used. Throughout his fellowship, Dave is working closely with four sexual health clinics in Wales (based in Aneurin Bevan UHB, Cardiff and Vale UHB, Betsi Cadwaladr UHB, and Swansea Bay UHB), a group of mentors with a wide range of expertise, and a stakeholder group comprising experts in PrEP use, PrEP prescribing, sexual health advocacy, and policy.
PhD studentship Funded By Pan-Wales Knowledge Exchange Skills Scholarship (KESS 2)

From PrEP’s initial release there has been concerns raised about how the protection provided from PrEP may result in a reduction in condom use. While the individual will be safe from contracting HIV, there are numerous sexually transmitted infections that can be caught and passed on. While at the moment it may be of little concern as individuals can just head to their local GUM clinic and receive treatment this may not always be the case. Antibiotic resistance is rapidly making our current antibiotics ineffective at treating STIs, particularly gonorrhoea. A reduction in condom use could lead to an increase in STIs with increased treatment resulting in antibiotics becoming resistant faster. It is essential that we understand how PrEP may be impacting peoples condom use behaviours. From this understanding appropriate measures can be implemented alongside the provision of PrEP to combat low condom usage. This PhD studentship is funded by the Knowledge Exchange Skills Scholarship (KESS 2) which is a pan-Wales higher level skills initiative led by Bangor University on behalf of the higher education sector in Wales. This initiative pairs students with external partners from Wales, for this project it is Public Health Wales.
PrEP Routinely Available Across Wales
And so we get to today when PrEP is now available as routine across Wales. Dave and Adam’s research is still ongoing and will inform the way services and support is delivered in Wales and more broadly. We also have new research questions that are coming through, including reach of services and issues around stigma and self-stigma. We are a part of the new Fast Track Cardiff and Vale initiative to deliver the UNAIDS 90/90/90 targets and reduce HIV stigma to zero. The learning from this can then be rapidly disseminated and implemented throughout Wales. Being a small country has allowed us to link closely policy, practice and research in a mutually supportive partnership that aims to deliver a step change in health to our country.
Related links
https://gov.wales/written-statement-availability-pre-exposure-prophylaxis-prep-prevent-hiv
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)00056-2/fulltext
- April 2024
- March 2024
- December 2023
- November 2023
- September 2023
- July 2023
- June 2023
- April 2023
- March 2023
- February 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- November 2021
- September 2021
- July 2021
- June 2021
- May 2021
- March 2021
- February 2021
- December 2020
- November 2020
- September 2020
- August 2020
- July 2020
- January 2020
- December 2019
- October 2019
- September 2019
- July 2019
- June 2019
- May 2019
- April 2019
- February 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- December 2017
- October 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- October 2016
- August 2016
- June 2016
- April 2016
- March 2016
- February 2016