NHS At 70: The Challenge of Reducing Health Inequalities Through Evidence Based Medicine
5 July 2018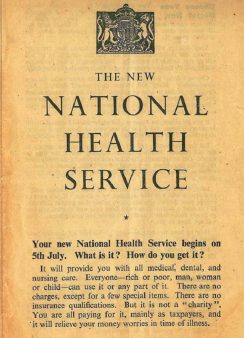
A New Beginning
In 1948, after a war which had rocked the world and challenged previous carefully drawn boundaries between genders, class and affluence, the belief that a better world could be built for all our children resulted in the National Health Service being born. It was born into a world where good medical care was available if you could pay for it and – if you didn’t – you got nothing. This was the same year that one of the most influential early randomised controlled trials was published in the Lancet. This trial showed that Streptomycin could improve outcomes for patients with TB and within a small number of years was completely changing the landscape of infectious disease treatment.
Where previously the focus was on detection and isolation (with bed rest) as the main treatment, we could now cure a previous often deadly disease (and one that my own grandfather succumbed to in 1950). This was one of the first of what has become the established approach to evaluating new treatments and, whilst the methods have developed, is one of the reasons we exist as a Centre for Trials Research today. The development and implementation of randomisation into our approach to testing has hugely improved on our ability to measure objectively the effects of new treatments.
Inverse Care Law

In 1971, on the NHS’s 23rd birthday, I was born in the Anwen Ward at Glangwili Hospital Carmarthen. My birth and childhood were rich in many things, but not money and, each time I stumbled and fell (which was a lot), the NHS was there to pick me up, x-ray me and patch me back together for no cost. I still enjoy the company of both of my parents today and in no small part that is also down to having a NHS that delivers care according to need rather than ability to pay. 1971 was also the year that Julian Tudor Hart (pictured above), a GP from the South Wales valleys, published a key paper in the Lancet which presented the concept of The Inverse Care Law: ‘the availability of good medical care tends to vary inversely with the need for it in the population it serves’. Even in a nationalised service it was recognised that there was a provision for all, but more was still provided to some than others, but this paper also recognised that the inequalities in delivery of health care would be even more pronounced if market forces were involved. After 23 years, it was clear how vitally important the NHS was, but also that it still had work to do to truly provide to all the people.
The availability of good medical care tends to vary inversely with the need for the population served. This inverse care law operates more completely where medical care is most exposed to market forces, and less so where such exposure is reduced. – Lancet 1971
Evidence Based Medicine
In 1996, the term Evidence Based Medicine was formally coined to define treating patients with the conscientious use of evidence on what worked and in 2002 Graham Watt followed up Julian Tudor Hart’s paper in the Lancet in 1971, noting that some particularly socially deprived communities seemed to be research-free zones and wondering on the impact this had on the generalisability of evidence. There have been many reviews since to show that there are populations who are typically research-excluded such as the elderly, children, those with low IQ, mental health problems, without capacity to consent; the list can go on and on.
Reducing Health Inequalities
The teams at the Centre for Trials Research work every day to provide evidence to improve cancer treatments, to support patients with neurodegenerative conditions, to improve public health, but if I was to say what I am most proud of in our portfolio it is the work we do to address health inequalities: to ensure that good research is done including and with people with learning disabilities, people in care homes, children in schools. In the era of Evidence Based Medicine it is only by providing strong inclusive evidence that we can even start to address the Inverse Care Law.
We need to ensure that not only does there continue to be a NHS, but that it truly is providing the best healthcare to all. The final words belong to its creator:
Not even the apparently enlightened principle of the ‘greatest good for the greatest number’ can excuse indifference to individual suffering. There is no test for progress other than its impact on the individual
– Aneurin Bevan 1952
In memory of Julian Tudor Hart (9 March 1927 – 1 July 2018).
- April 2024
- March 2024
- December 2023
- November 2023
- September 2023
- July 2023
- June 2023
- April 2023
- March 2023
- February 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- November 2021
- September 2021
- July 2021
- June 2021
- May 2021
- March 2021
- February 2021
- December 2020
- November 2020
- September 2020
- August 2020
- July 2020
- January 2020
- December 2019
- October 2019
- September 2019
- July 2019
- June 2019
- May 2019
- April 2019
- February 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- December 2017
- October 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- October 2016
- August 2016
- June 2016
- April 2016
- March 2016
- February 2016